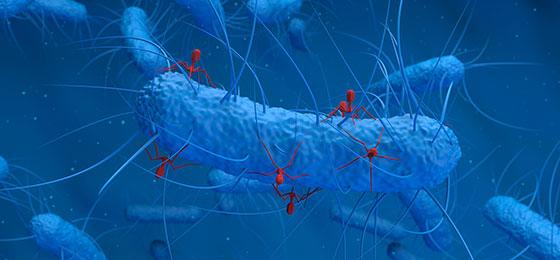
Phages: more versatile than previously thought
Phages kill bacteria. But in the process, they can also spread antibiotic resistance. New findings reveal dangers - and opportunities for medicine.
Portrait / project description (completed research project)
Bacteriophages (short: phages) are viruses that infect and kill bacteria. For some time, research has been conducted into using them specifically to treat bacterial infections. But phages not only kill bacteria, they can also transfer antibiotic resistance genes from one bacterium to another: When multiplying in the cells of targeted bacteria, they inject their own genetic material into new virus particles, and in some cases also add genetic material from the host bacteria – sometimes, this can be a resistance gene. If one of these viral particles then infects a new bacterium, the resistance may be transferred. However, this mechanism has received little attention regarding the spread of antibiotic resistance to date, and little is known about the role phages - the most abundant biological entities on earth - play in the spread of antibiotic resistance across humans, animals and the environment.
Wastewater: A treasure trove for a wide variety of phages
Elena Gomez Sanz and her team at ETH Zurich have now investigated these processes in more detail - and made some surprising discoveries. Up to now, it was widely assumed that specific phages can only infect very specific bacteria. This would narrow their scope of impact and act as a natural barrier for the phage-mediated spread of genetic material, and thus antibiotic resistance. While Staphylococcus aureus (the best-known species of the genus) has been for long subject of studies on this form of gene transfer, research has primarily worked with samples from human medicine and identified phages that are of immediate clinical relevance.
In contrast, Elena Gomez Sanz and her team searched for as many different natural Staphylococcus phages as possible in their project. They found these in wastewater, where a great diversity of bacteria and their phages converge – from humans, animals, households, industry and agriculture. The researchers were able to isolate almost a hundred different types of phages from wastewater for their project. They then conducted laboratory experiments to test which bacteria these phages infect, using nearly 120 bacterial strains, covering 29 staphylococcal species.
Phages attack more different bacteria than previously thought
Contrary to previous assumptions, it was shown that phages can attack not only one bacterial species, but on average four different ones. The researchers observed numerous different combinations of targets, so that “shared” phages may enable one staphylococcal species to exchange genetic material with, on average, seventeen other species. They also conducted an experiment in which they introduced a previously absent natural mobile resistance gene into one of the bacteria tested. It turned out that phages also incorporated this into new virus particles. These results prove that phages create widely branched connections through which antibiotic resistance can spread between bacterial species, across the entire biological system of humans, animals and the environment. This knowledge is of great importance for further research on the spread of antibiotic resistance. At the same time, it highlights the need of the efficient removal of phages in wastewater treatment.
Furthermore, the teams’ findings are crucial regarding the use of phages to combat pathogenic bacteria in humans. The discovery that phages can have a broad host range makes it easier to use them against many different bacteria. On the other hand, however, when using phages in medicine, one must be careful that they don’t unintentionally transmit antibiotic resistance genes. Drug developers thus have to pay close attention to the exact propagation mechanism of phages used in medicine.
May 2022
Original title
Insights into the role of phages on the bacterial resistome
